Abstract
Background: Advances in supportive care and novel therapies have driven improved outcomes for patients with Multiple myeloma (MM) and Light Chain Amyloidosis (AL). Unfortunately, this progress demands a heavy toll - higher patient costs. Financial toxicity (FT) is the adverse impact of cancer on a patient's financial well-being, contributing to increased distress, lower medication compliance, and even reduced survival. We aimed to evaluate MM and AL patients for financial toxicity over time to better understand its impact on various quality of life (QOL) domains.
Methods: Adult patients with MM or AL that receive care at Mayo Clinic, Rochester MN, were recruited for a prospective study between December 2019 and March 2021. FT was measured using the validated COmprehensive Score for financial Toxicity (COST) questionnaire at the time of enrollment, 3 months, and 6 months follow-up. COST scores range from 0-44, with higher scores indicating lower FT. We defined patients with a COST score of ≤ 23 as having substantial FT. Domains of QOL were assessed via the Patient Reported Outcome Measurement Information System (PROMIS)-29 survey. Patient demographics and clinical information were abstracted from the electronic medical record. Statistical analysis included a comparison of COST scores among groups through Wilcoxon rank-sum, Kruskal-Wallis, and Jonckheere-Terpestra tests for binary, unordered, and ordered categorical variables, respectively.
Results: One hundred and sixteen patients (96 MM, 83%; AL 20, 17%) enrolled in this study. The cohort is characterized as follows: 49% age 65+ (51% age 35-64), 54% male, 93% White, 4.3% Black, 3.5% Hispanic, 44% with incomes > USD 75k/yr (26% < USD 50k/yr), 77% with at least some college education (32% graduate or doctoral degree), 52% insured through Medicare (4.3% through Medicaid), 36% employed (53% retired), and 71% married (16% divorced). Forty-three percent of patients enrolled in the study were newly diagnosed (56% relapsed), and 72% had received an autologous stem cell transplant.
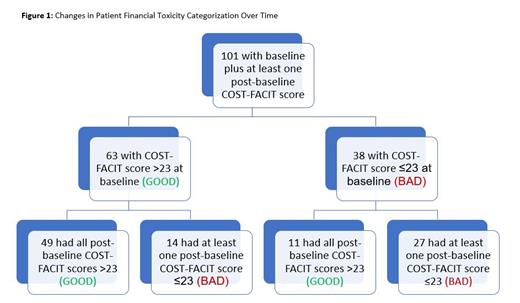
Baseline mean COST score was25.9 (N=116; SD 10.2), with 37% reporting FT. A total of 101 patients (85 MM; 16 AL) completed a baseline and either 3- or 6-month COST survey. Thirty-eight of these patients (38%) reported FT at the time of enrollment. Among those reporting baseline FT, 71% continued to report FT at 3 or 6 months; 29% showed reduced FT. Of the 62% of patients who reported low FT at baseline, 78% showed continued low FT at 3 or 6 months; 22% showed increased FT. Results of longitudinal follow-up are outlined in Figure 1. FT was significantly associated with increased anxiety, depression, and pain intensity domains on the PROMIS-29. Substantial FT was associated with: women, Medicaid as primary insurance, and being divorced. FT was also greater in unemployed/disabled vs retired individuals. Conversely, low FT was associated with: males, earning > USD 75k/yr, Medicare as primary insurance, having at least some college education, being retired, and traveling 300+ miles for care. Financial toxicity did not differ significantly by age, race, ethnicity, disease status (newly diagnosed vs relapsed), or transplant status.
Discussion: Financial toxicity was present in more than one-third of AL and MM patients in this high-earning and well-educated cohort. Financial toxicity was associated with increased anxiety, depression, and pain intensity, contributing to lower patient quality of life. Longitudinal follow-up has shown financial toxicity to be dynamic, necessitating routine evaluation of patient financial burdens. Future work will focus on automating FT assessment with incorporation into routine care and developing care processes to support patients.
Dispenzieri: Alnylam: Research Funding; Takeda: Research Funding; Pfizer: Research Funding; Oncopeptides: Consultancy; Sorrento Therapeutics: Consultancy; Janssen: Consultancy, Research Funding.